In recent years, the connection between stress and diabetes has emerged as a subject of extensive research and discussion within the medical community. While stress, in itself, has been a recognized concern for decades, understanding its direct influence on conditions such as diabetes offers a new perspective on healthcare.
For many, the question, “can stress cause diabetes?” has become more than just a curious thought. It’s a real concern rooted in observed patterns. For instance, consider Jane, a 60-year-old retiree. She led a relatively healthy life but noticed sudden spikes in her blood sugar levels during particularly stressful periods – like when she moved to a new city or faced family challenges. She isn’t alone. Many report fluctuations in their blood glucose during times of emotional stress, whether it’s stemming from financial worries, health scares, or even relationship troubles.
Medical professionals are noting these patterns too. An elevated stress level, be it due to psychological stress or physical stress, has demonstrable effects on the body’s metabolism. The release of stress hormones, especially glucocorticoids, impacts how the body manages its blood sugar. Over time, such hormonal and metabolic responses can contribute to conditions like chronic stress-induced hyperglycemia.
To simplify, imagine the body as a well-calibrated machine. Just as a car might stutter or stall when there’s an issue with its fuel or engine, our bodies show signs – like fluctuating blood sugar levels – when there’s a disturbance in its usual rhythm, often due to intrinsic or external stimuli like stress.
This raises the essential question: if stress plays such a pivotal role in influencing blood sugar levels, how can individuals and healthcare professionals proactively manage and monitor it?

Life Transitions and Their Stressors
Life is a series of transitions. As we age, we’re bound to encounter various milestones and challenges, from retirement and health changes to shifts in family dynamics or residence. While these events are often seen as a natural progression, they can bring about considerable stress, even if we don’t always recognize it immediately.
It’s crucial to understand that our bodies have a physiological response to these stressors. The body’s fight or flight response is triggered more often than we might realize. When confronted with stress, be it due to significant life changes or even daily hassles, our bodies release a cascade of stress hormones.
Continued exposure to these hormones, especially during prolonged periods of stress, can lead to high blood pressure and chronic stress-induced hyperglycemia. This condition means that even if an individual does not have a history of diabetes, the persistent stress and the subsequent release of glucocorticoids can disrupt their normal blood glucose levels.
Moreover, the risks aren’t just physiological. Chronic stress, if not addressed, can lead to behavioral changes, such as unhealthy diet patterns or reduced physical activity, both of which can further exacerbate blood sugar discrepancies.
In a nutshell, life’s transitions, though often inevitable, bring about a cascade of effects on our wellbeing. Recognizing the signs, understanding the physiological implications, and adopting strategies to cope can make all the difference in ensuring these transitions don’t adversely impact our health.

The Body’s Stress Response Over Time
Every individual, at some point in their life, will face stress. However, the body’s response to stress isn’t static; it evolves over time, influenced by factors like age, experiences, and overall health. As we age, it becomes increasingly essential to recognize how our body’s reaction to stress shifts and the implications of these changes.
When stress is encountered, the body activates its innate fight-or-flight response. This ancient mechanism equips us to handle immediate threats. The heart rate quickens, muscles tighten, and there’s a rush of adrenaline.
In younger years, once the immediate threat or stress has passed, the body usually returns to its baseline state relatively quickly. However, as we progress in age, the body’s efficiency in this recovery process might decrease. The stress hormones that once were swiftly cleared from the system might linger for longer, causing prolonged elevation in blood sugar levels.
Chronic stress over time can lead to a state of continuous elevation in glucose, known as chronic stress-induced hyperglycemia. Unlike the acute spikes that might be seen with immediate stressors, this state means the body remains in a heightened state of alert, leading to disturbed glucose homeostasis.

Embracing the Power of Continuous Glucose Monitoring (CGM)
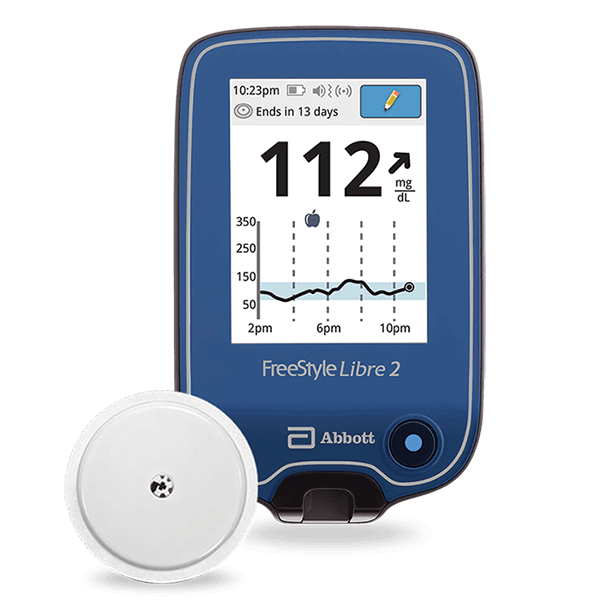
Blood sugar management is a foundational pillar for those conscious of their health, particularly in the context of advancing age and the increasing complexities it brings. A breakthrough in this domain has been the Continuous Glucose Monitoring system or CGM. Let’s dive deeper into its workings and its profound implications for stress-induced blood sugar fluctuations.

Understanding the Mechanics of CGM
How Does A Continuous Glucose Monitor Work? CGM stands out as a marvel of medical technology. Instead of the sporadic readings obtained from traditional glucose meters, which often feel like trying to understand a story from random chapters, CGM provides a continuous narrative of glucose levels. It comprises a sensor, typically implanted under the skin, which measures glucose in the interstitial fluid. These measurements are then relayed to a device or smartphone, providing almost real-time readings.

Why Every Fluctuation Matters
Life is a series of events, and for someone keen on understanding their body’s responses, especially in relation to stress, every glucose fluctuation is a clue. Stressful events, both psychological and physical, can lead to sudden spikes or prolonged elevations in blood sugar. However, with CGM, not only can one witness these fluctuations, but one can also tie them back to specific triggers, enhancing self-awareness and prompting proactive interventions.
As the years progress, the body’s responses, including its blood glucose regulation, undergo changes. This is where CGM offers tailored advantages:
Safety Nets: Many CGMs have alert systems that signal when glucose levels breach set thresholds. This is particularly valuable for individuals who might be less sensitive to the symptoms of hypoglycemia or hyperglycemia.
Trend Analysis: Beyond immediate readings, CGMs provide trend data, illuminating patterns that might be linked to meal timings, medications, or daily routines. This aids in making more informed adjustments to one’s regimen.
Remote Monitoring: Some advanced CGM systems allow for remote monitoring by caregivers or medical professionals, ensuring an added layer of safety and support.
Mindfulness and Meditation: Grounding oneself in the present moment can help alleviate the burdens of the past and the anxieties of the future. Regular meditation, even if for just a few minutes a day, can significantly reduce perceived stress levels.

Physical Activity: Exercise is a double-edged sword against stress. Not only does it consume the extra glucose produced during stressful situations, but it also releases endorphins, which are natural mood lifters.

Balanced Diet: Eating a well-rounded diet with a focus on whole foods and avoiding excessive caffeine and sugar can help regulate blood sugar and improve the body’s response to stress.
Limit Stimulants: Reducing or eliminating the consumption of stimulants, such as caffeine and nicotine, can help in keeping stress and, consequently, blood sugar levels in check.

Deep Breathing and Relaxation: Techniques like deep breathing, progressive muscle relaxation, and visualization can aid in immediate stress relief by activating the body’s relaxation response.

Medicare and the Avenue to Modern Monitoring
The transformative potential of CGM hasn’t gone unnoticed. Medicare, in its bid to offer beneficiaries the best possible care, covers certain CGM systems. To be eligible, individuals need to meet specific criteria, predominantly those who require multiple daily injections of insulin or use an insulin pump. Partnering with healthcare providers can streamline the process, ensuring that those who stand to benefit the most from CGM have it within their grasp.
In sum, CGM isn’t just a technological tool; it’s a paradigm shift in the realm of health monitoring. As stress and its multifaceted effects on blood sugar take center stage, embracing CGM offers not just a reactive solution but a proactive strategy to steer one’s health journey confidently.
Managing Stress to Control Blood Sugar
Stress, in its myriad forms, can stealthily undermine even the most robust health regimens. Especially concerning is its profound effect on blood sugar, a relationship that’s both direct and complex. Let’s delve into the means through which stress can be managed to ensure blood sugar remains in check.

Understanding Stress and Its Impact
Stress is the body’s natural reaction to intrinsic or external stimuli, ranging from immediate threats to long-term challenges. While the short-term “fight or flight” stress response can be beneficial in some circumstances, chronic stress has cumulative effects, including persistent elevations in blood glucose levels.
When under stress, the body releases stress hormones like cortisol and adrenaline. These hormones prompt the liver to produce more glucose, the body’s primary source of energy, to prepare for the perceived threat. However, without the corresponding physical activity to use this extra energy, blood sugar levels can remain elevated.
Practical Stress Reduction Techniques
Managing stress isn’t about eliminating it but learning how to respond to it more healthily. Here are some practical approaches:

Mental Health and Its Role in Stress Management
It’s vital to recognize that managing stress is intertwined with overall mental well-being. Anxiety, depression, and other mood disorders can amplify the body’s stress responses. Seeking support, be it through therapy, counseling, or support groups, can provide tools and perspectives that are invaluable in the stress management journey.

The Power of Routine
Establishing a daily routine, including set meal times, regular exercise, and dedicated relaxation periods, can provide a sense of normalcy and predictability. This structure can be especially comforting in turbulent times and can help mitigate the roller-coaster effects of erratic blood sugar levels.
In essence, the nexus between stress and blood sugar is intricate, but with informed interventions and proactive measures, one can navigate life’s challenges while maintaining optimal blood glucose levels.

Stress, Blood Sugar, and Total Wellness
The intricate interplay between stress and blood sugar underscores the vast implications of our emotional and physiological responses over time. Chronic stress, left unchecked, has the potential to amplify disturbances in glucose homeostasis, escalating more profound health challenges over time. Delving deep into the relationship between these factors isn’t just a dialogue on diabetes management—it’s about holistic health and wellness.
The mechanisms through which stress modifies blood sugar levels—like the surge of stress hormones and their subsequent impact on glucose production—are undoubtedly intricate. Yet, the solutions can be quite direct and readily available. Incorporating stress-reducing practices, understanding the profound benefits of tools like Continuous Glucose Monitoring (CGM), and seeking appropriate medical and mental health assistance are invaluable steps towards healthier blood sugar management.
In this context, it’s imperative to highlight the progressive solutions offered by Aptiva Medical. Our state-of-the-art CGM systems are not just tools but allies in your journey towards better health. Designed with the user’s needs in mind, CGM devices empower individuals with real-time data, providing insights that can be life-changing.
Remember that each individual’s journey with stress and its effect on blood sugar is personal. What’s effective for one person may differ for another. Continuous self-awareness, monitoring, and proactive management hold the key.

Don’t wait for tomorrow. Equip yourself with the knowledge, tools, and techniques to manage stress and monitor blood sugar effectively. Explore Aptiva Medical’s advanced CGM systems, tailored to offer you the insights you need. Because you deserve health solutions that are as dynamic as your life. Dive deeper into what Aptiva Medical has to offer and take control of your well-being today.