Continuous glucose monitoring (CGM) is a relatively new way to track your blood sugar levels. Instead of getting snapshots of a few moments – moments which could be influenced by a multitude of factors – you can see your glucose levels changing throughout the day. You can analyze trends to learn what’s affecting them and make proactive and long-term treatment decisions to ultimately live a longer and more able-bodied life.
What is continuous glucose monitoring (CGM)?
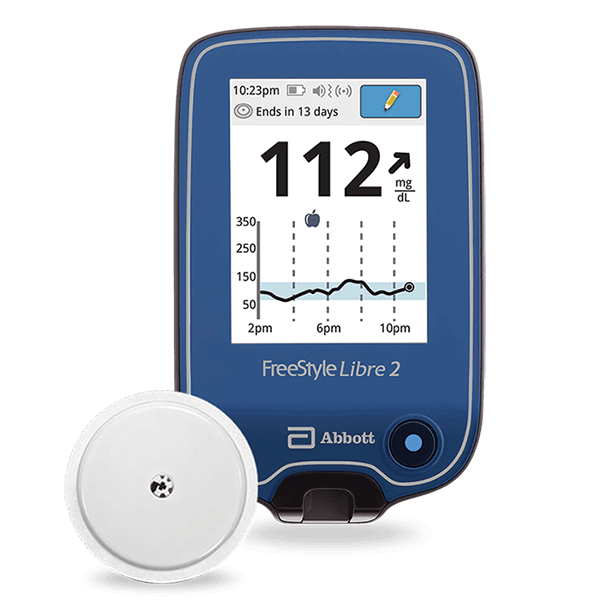
Continuous glucose monitoring is a small device that attaches to your skin with medical adhesive. A sensor inside the device monitors your glucose levels so you can see changes before they become a problem. Some CGM systems record your glucose readings so you can track trends and improve your overall health with tight blood sugar control.

CGM systems are only available by doctor’s prescription. When you and your doctor decide to add a CGM device to your treatment plan, they provide the information you need to get started. They may even bring you back to the office when you receive your CGM system to walk you through the initial setup. Setup typically involves:
sensor insertion
calibration
setting thresholds for alerts
data transfer settings
establishing treatment responses based on new real-time data
But before you talk to your doctor about getting a CGM system, you might want to understand how they work and what you can expect when using one. Keep in mind every model is slightly different. Some don’t require calibration. Some sensors last longer than others. Some work with your smartphone.
Generally speaking, a continuous glucose monitor comes with two to four parts:
applicator
sensor
transmitter
receiver
You might have all four, or you might have an applicator and a sensor/transmitter combo that works with your smartphone or another smart device.
CGM works like this:
1. You insert the sensor.
Most CGM systems come with an applicator. The applicator makes it fast and easy to insert the sensor in three steps:
Put the sensor in the applicator.
Choose a sensor location on your skin.
Place the applicator and push the button.
Applicator instructions may vary by manufacturer. Be sure to read the instructions that come with your system. The instructions will also tell you what locations are best for the sensor. Once placed, the sensor is held in place by medical tape, which should be included in the package.
2. The sensor will measure your glucose levels.
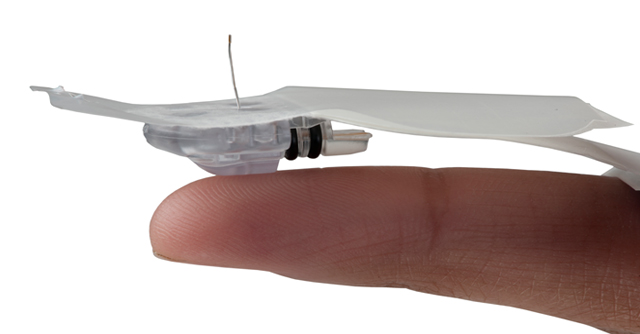
CGM measures the glucose levels in your interstitial fluid with a tiny filament in the small sensor. Interstitial fluid is the fluid surrounding the cells under your skin. This is not the same as a blood glucose reading, but it can tell you that your blood glucose levels are changing before they get too high or low. That’s because your interstitial fluid comes from your capillaries.

3. The transmitter sends data to the receiver.
Your sensor continuously measures and sends glucose data to the receiver via the transmitter. In some models, the transmitter and sensor are combined in one assembly. In other models, the transmitter is a separate piece that you’ll attach to each replacement sensor individually.

4. You read and respond to your data.
You’ll receive your glucose level data on the receiver that comes with your CGM system or on your smartphone or another smart device. Being able to see your real-time glucose levels throughout the day and night allows you to make proactive treatment decisions and improve your overall health.
The receiver also allows you and your doctor to download your data. You can view trends and learn everything there is to know about your unique responses to stimuli. Together with this information, you and your doctor can create a better diabetes care plan to improve glycemic control.
5. You change your sensor every 14 days or so.
Depending on the model you choose, your sensor will need to be changed every ten to 14 days. There are some long-term devices that are only changed a few times a year, but those sensors have to be inserted and replaced by your physician.

Benefits of using CGM to monitor blood glucose levels
1. Continuous glucose monitoring makes it easier to stay in range.
You’ve probably spoken to your doctor about the importance of keeping your blood glucose within a healthy range. A typical goal is between 70 and 180 mg/dL. Traditionally, you don’t know that you’re getting out of that range until you test yourself or start showing symptoms. By the time you have symptoms, your health is already compromised.
The Endocrine Society recommends:
Less than one hour per day below 70 mg/dL
Less than 15 minutes per day below 54 mg/dL
Less than six hours per day above 180 mg/dL
less than 10 minutes above 250 mg/dL
Total Time in Range (TIR) over 17 hours per day
They also state that TIR targets might be lower for older or high-risk patients.
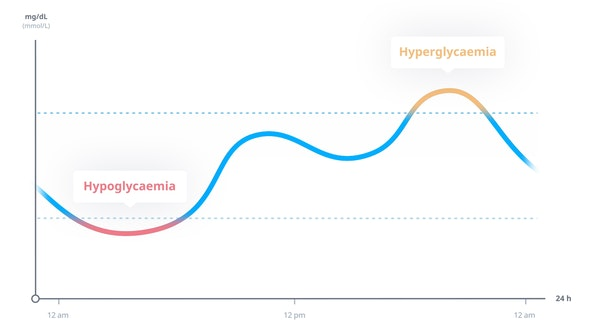
What is time in range (TIR)?
Time in Range is the percentage of the day that your blood glucose is within your target range. For the recommendation from the Endocrine Society (17 hours per day), the TIR would be written as 70% (17 out of 24 hours).
The American Diabetes Association states that you’re less likely to have diabetes complications like digestive and kidney diseases if you spend more time in range. That’s why TIR and continuous glucose monitoring are quickly becoming the leading methods of informing your diabetes treatment plan. The National Institute of Diabetes and Digestive and Kidney Diseases credits CGM with “fewer low blood glucose emergencies.”
2. Learn how different foods, physical activity, sleep, illness, and stress affect your blood sugar levels.
Continuous glucose monitoring gives you blood glucose readings all day, day and night. Without pricking your fingers or testing, you can see exactly how different factors affect your blood sugar. With that priceless information, you can make choices that give you a longer and happier life.

3. Help your doctor help you.
Your doctor can download your glucose levels directly from your CGM. Then they can analyze your trends and levels to provide better, more personalized diabetes care.
4. Address issues quickly – before you’re at risk.
We know that a higher TIR reduces your risk of developing potentially serious diabetes complications. You can set your continuous glucose monitoring (CGM) device to alert you when your blood sugar levels get too high or too low – before you’re actually out of your target range. Then you can make quick treatment decisions that ultimately have a critical impact on your health.

5. Everyone’s favorite – fewer fingersticks.
Think of all the times you’ve used a blood glucose meter just to find out you don’t need to make any changes to your regular regimen. With continuous glucose monitoring, you can just check your levels on your smart device or CGM receiver. The only time you’ll need to poke your finger is when you’re having symptoms or when your CGM system gives a reading that requires treatment.

The dangers of hypoglycemia unawareness
CGM is more than convenient. It’s a more reliable method of preventing high or low blood glucose. Low blood glucose is dangerous because it increases your risk of complications and drastically reduces your health over time. Not knowing that your blood sugar is low puts you at risk of severe hypoglycemia, which can be fatal.
Can you throw away your glucose meter?
No. As much as you might enjoy tossing your meter, it’s still a vital part of your diabetes treatment. Before you respond to CGM results with insulin or sugar, you should verify your CGM reading by using your blood glucose meter.

What’s the difference between blood sugar and interstitial fluid glucose levels?
The glucose levels read by your CGM system are directly related to your blood sugar levels. The fluid between your cells comes from your capillaries, which contain blood. By watching glucose trends in your subcutaneous fluid, you can see how your blood sugar is changing.
Is continuous glucose monitor the same as an insulin pump?
No. A CGM system only monitors your glucose level. A continuous insulin pump is a separate device that delivers insulin injections. Insulin pumps don’t monitor your blood sugar; they just reduce the need for manual insulin shots with automated insulin delivery. They are similar in that they each have a wearable device and function automatically.

What is an artificial pancreas?
An artificial pancreas is a continuous glucose monitor and insulin pump that communicate with each other. The monitor tells the pump how much insulin you need and when to inject it. This system is best for people who are on intensive insulin therapy or injecting insulin several times a day.

Do continuous glucose monitors have a needle?
Kind of. Placement of the sensor works like an IV, an intravenous catheter used to deliver fluid and medications. A needle is inserted into the skin. The needle has a tiny filament inside. The needle is removed, and the filament stays in. These two steps happen quickly and automatically when you use a CGM applicator.

How does a CGM attach?
Most CMG systems come with an applicator. The applicator is usually a small device with a button. The CGM sensor is inside the applicator. You place it against your skin, push the button, and the sensor is attached. The applicator detaches when the sensor is placed.
Why do people stop using CGM?
A 2018 study conducted by GlySens Inc surveyed 1,348 respondents to discover their reasons for quitting their CGM usage. Two of the top five reasons given by adults were “too expensive” and “not covered by insurance.” The other top five reasons were that the sensor was uncomfortable, they had too many alerts, and they believed the data wasn’t as accurate as their SMBG.
What are the contraindications for blood glucose monitoring?
A comprehensive study of the effects of CGM conducted in 2013 by the German Diabetes Association revealed the following contraindications – meaning these factors do not predict success with CGM devices:
lack of motivation and compliance
fear of technology/lack of trust in technology
alcohol and drug abuse
unrelated psychological conditions like psychoses or eating disorders

How much does a CGM system cost?
Prices vary per brand. Typical prices for the Dexcom G6:
$400 for the receiver
$300 for the transmitter
$420 for a month’s worth of sensors
These prices are prohibitive for many people with type 1 diabetes, but patients with a Medicare health insurance plan can typically get their CGM system for no out-of-pocket costs. Medicare actually prefers to cover the costs because they save money in the long run when they help their recipients manage diabetes better.