Gestational diabetes, a condition that emerges during pregnancy, has become a prevalent concern among expecting mothers. It uniquely affects pregnant women, even those who haven’t had a prior history with diabetes. When a woman develops high blood sugar levels during her pregnancy, she’s grappling with gestational diabetes. This temporary diabetic phase, if not appropriately addressed, could lead to an array of health problems for both the mother and her baby. Thus, it becomes essential to understand its nuances, how it affects pregnancy, and the ways in which one can monitor and manage it. In this comprehensive guide, we’ll dive deep into what gestational diabetes is, how it’s diagnosed, its impacts, and the crucial steps one can take to ensure the health and well-being of both the mother and the baby. Whether you’re an expecting mother, a partner, a family member, or just someone eager to learn, this blog will provide insights to help you grasp the essentials of gestational diabetes.
Understanding Gestational Diabetes
Gestational diabetes mellitus (GDM) is a form of diabetes that specifically emerges during pregnancy. It’s a condition where the body cannot make or use all the insulin it needs, resulting in elevated blood sugar levels. Insulin is a hormone that helps your body regulate the amount of sugar in your blood. During pregnancy, a variety of hormonal changes occur, and some of these hormones can lead to insulin resistance.
But what exactly is insulin resistance? At its core, insulin resistance is when cells in the muscles, fat, and liver don’t respond well to insulin and can’t easily absorb glucose from the bloodstream. As a result, the pancreas produces more insulin to help glucose enter cells. For many pregnant people, the body can cope with this by producing more insulin. However, for some, this increased demand isn’t met, leading to the glucose buildup in the bloodstream, hence gestational diabetes. NIDDK offers more in-depth insights into how the body manages increased insulin demand.
So, why is it vital to discuss gestational diabetes? For starters, this condition can lead to both short-term and long-term health complications. In the short term, unmanaged gestational diabetes can result in the baby growing too large, leading to complications during delivery, premature birth, and respiratory distress syndrome among other issues. In the longer term, both the mother and the child can have a higher risk of developing type 2 diabetes later in life.
It’s also worth noting that while any pregnant woman can develop gestational diabetes, certain risk factors can elevate the chances. These include a family history of diabetes, being overweight before pregnancy, having polycystic ovary syndrome, or having had gestational diabetes during a previous pregnancy. Additionally, age plays a role; women who are over the age of 25 are at a higher risk.
What’s both intriguing and challenging about gestational diabetes is its sneakiness. Often, gestational diabetes symptoms are subtle and can mimic regular pregnancy symptoms. This is why the American Diabetes Association recommends all pregnant women get screened for this condition, typically with an oral glucose tolerance test.
It’s not all gloomy, though. With careful control, a balanced diet, regular check-ups, and the right treatment, most women with gestational diabetes can have a healthy pregnancy and a healthy baby. The key is understanding the condition, its risks, and the many ways to manage it.

Diagnosing Gestational Diabetes
Diagnosing gestational diabetes is paramount to ensuring the health and well-being of both the mother and the baby. Accurate diagnosis allows for timely management and reduces potential health complications. But how is gestational diabetes diagnosed, and what does the process entail?
For starters, pregnant women usually undergo screening for gestational diabetes between 24 and 28 weeks of pregnancy. This is typically the time frame when gestational diabetes first starts to manifest, although it can vary among individuals. Here’s a closer look at the diagnostic procedures:
- Glucose Challenge Test (GCT): This initial screening test involves drinking a sugary solution, followed by a blood test an hour later. The primary aim of this test is to check how the body processes sugar. It doesn’t necessarily diagnose diabetes but identifies those who may be at risk and need a more definitive test.
- Oral Glucose Tolerance Test (OGTT): If the results from the GCT indicate high blood sugar levels, an OGTT will be the next step. The procedure begins after an overnight fast. The pregnant individual will have a baseline blood sample taken, then drink a glucose-rich drink, much denser than the one taken during the GCT. Blood samples are then taken every hour for 2 to 3 hours. High blood sugar levels in two or more samples would typically mean a gestational diabetes diagnosis.
It’s essential to understand that while these tests might sound intimidating, they are standard procedures and are a crucial step in ensuring the baby’s health and the mother’s overall health. They’re also incredibly reliable, with the oral glucose tolerance test being considered the gold standard in diagnosing gestational diabetes. For more on this diagnostic approach, the Mayo Clinic provides a detailed overview.
Certain factors might influence the accuracy of these tests. For instance, not adhering to the pre-test conditions, like eating when you should be fasting, can skew results. It’s vital to follow medical guidance closely.
Risk factors play a pivotal role in determining how closely healthcare providers might monitor a pregnant individual. Those with a history of diabetes, a high BMI, previous large babies, or who had gestational diabetes in a previous pregnancy might undergo screenings earlier or more frequently.
Impacts of Gestational Diabetes
Gestational diabetes, while a temporary condition, can have significant consequences for both mother and child if left unchecked. The body’s inability to manage blood sugar levels effectively during pregnancy not only influences the pregnancy’s progression but can also create long-term health concerns. Exploring these impacts offers a comprehensive perspective on why managing gestational diabetes is of the utmost importance.

For the Mother:
- High Blood Pressure: One of the most common complications associated with gestational diabetes is high blood pressure. This condition can strain the heart and kidneys, leading to potential problems like preeclampsia, a serious pregnancy complication characterized by high blood pressure and potential damage to organs such as the liver and kidneys.
- Future Diabetes Risk: Women diagnosed with gestational diabetes have a higher risk of developing type 2 diabetes later in life. Regular screenings after pregnancy become crucial, and maintaining a healthy lifestyle can help in reducing this risk.
- Delivery Complications: High blood sugar levels can lead to the baby growing larger than average, which may result in the need for a cesarean section or other medical interventions during childbirth.
- Emotional Impact: Being diagnosed with gestational diabetes can be overwhelming, leading to feelings of guilt, anxiety, or fear. Proper support and understanding can help address these emotions.

For the Baby:
- High Birth Weight: Babies born to mothers with unmanaged gestational diabetes can be larger than normal, a condition termed ‘macrosomia’. This might lead to complications during delivery, including birth injuries.
- Low Blood Sugar (Hypoglycemia): After birth, the baby’s blood sugar level might drop significantly, leading to hypoglycemia. This can be a concerning situation, necessitating immediate medical attention.
- Respiratory Distress Syndrome: Babies might experience breathing difficulties if born prematurely, a potential result of gestational diabetes. They may require assistance with breathing until their lungs mature.
- Risk of Future Health Problems: Children of mothers with gestational diabetes have an increased risk for obesity and type 2 diabetes later in life. They may also be at a higher risk for heart disease and other related health problems.
- Birth Defects: Although less common, there is a heightened risk for birth defects, especially if the mother’s blood sugar levels are not well-controlled in the early stages of pregnancy.
- Jaundice: Babies born to mothers with gestational diabetes are more likely to develop jaundice, a condition where the skin and eyes display a yellowish tint due to high levels of bilirubin. It’s essential to monitor and treat jaundice promptly to prevent further complications.
In essence, gestational diabetes affects both the mother’s and the baby’s health in multiple ways, emphasizing the importance of early detection, rigorous monitoring, and appropriate management. Through knowledge, support, and proactive healthcare, many of the risks associated with gestational diabetes can be mitigated, paving the way for a healthy pregnancy and a thriving newborn.
Management and Monitoring of Gestational Diabetes
Proper management and consistent monitoring of gestational diabetes are paramount not only for the well-being of the mother but also for ensuring a healthy environment for the baby. A multifaceted approach, blending dietary modifications, physical activity, and potential medical treatments, can successfully navigate this health challenge.

Dietary Changes:
- Balanced Diet: Embracing a diet rich in nutrients and low in processed sugars and fats is crucial. Consulting a dietitian can provide personalized meal plans tailored to individual needs. Eating healthy foods, in correct proportions, can help maintain blood sugar levels within a normal range. For more on dietary recommendations during pregnancy, check out guidelines from USCF Health.
- Carbohydrate Counting: Keeping a tab on carbohydrate intake can aid in regulating blood glucose levels. Carbohydrates have a direct influence on blood sugar, and understanding how much to consume can keep fluctuations in check.
- Avoiding Sugary Beverages and Snacks: Sugary drinks and snacks can cause a rapid spike in blood sugar levels. Replacing them with healthier alternatives or consuming them in moderation is advisable.

Physical Activity:
- Regular Exercise: Engaging in moderate physical activity, such as walking or swimming, can help in managing blood sugar levels. However, it’s essential to consult with a healthcare provider to determine safe and suitable exercises during pregnancy.
- Weight Management: While weight gain is expected during pregnancy, excessive weight gain can exacerbate gestational diabetes symptoms. Staying within the recommended weight gain range ensures better blood sugar control.

Medical Interventions:
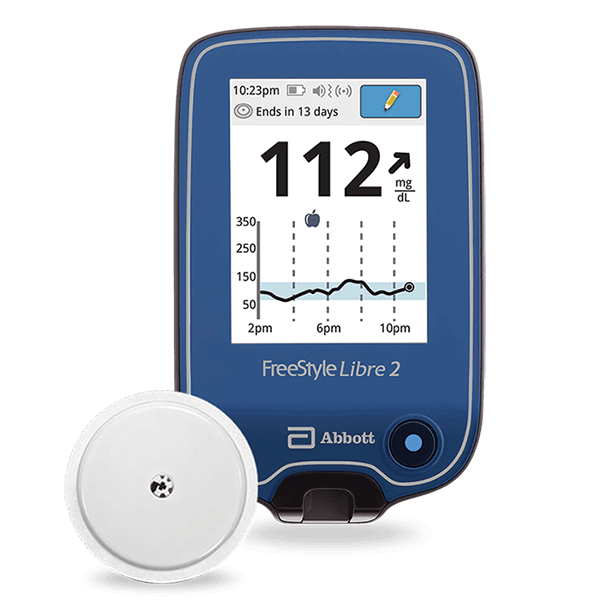
- Blood Sugar Monitoring: Regularly checking blood sugar levels becomes indispensable when diagnosed with gestational diabetes. The Centers for Disease Control and Prevention (CDC) provide further details on the importance of monitoring for pregnant women with this condition. Devices like glucometers and continuous glucose monitors (CGMs) can provide real-time feedback, allowing for timely interventions if levels stray from the healthy range.
- Insulin Injections: If diet and exercise are insufficient in maintaining blood glucose levels, insulin injections might become necessary. Insulin helps the body utilize glucose more effectively, overcoming insulin resistance encountered during pregnancy.
- Oral Medications: Some pregnant individuals might be prescribed oral medications to control blood sugar. However, this is less common than insulin therapy.

Use of CGM Systems:
- Continuous Glucose Monitoring (CGM): CGMs, such as those offered by Aptiva Medical, offer an advanced method to keep a vigilant eye on blood sugar fluctuations. These devices measure glucose in the interstitial fluid, giving frequent readings throughout the day and night.

The Advantages of Continuous Glucose Monitoring (CGM)
Continuous Glucose Monitoring (CGM) systems have dramatically revolutionized the way gestational diabetes and other forms of diabetes are managed. As the name suggests, CGM provides round-the-clock surveillance of blood glucose levels, offering insights and alerts that intermittent checks cannot. Here’s a closer look at why CGM during pregnancy stands out:
- Real-time Feedback: One of the hallmarks of CGM is its ability to provide immediate data on blood glucose levels. This real-time feedback allows individuals to see how certain foods, activities, or stresses influence their levels, helping them make informed decisions throughout the day.
- Trend Analysis: Beyond just the current blood sugar level, CGM devices display trends, showing whether glucose is on the rise, stable, or dropping. This predictive insight can be invaluable, especially for anticipating and preventing instances of very high or low blood sugar.
- Customizable Alerts: The system can be programmed to sound alarms or send notifications if glucose levels breach pre-defined thresholds. Whether it’s an impending instance of low blood sugar in the middle of the night or an unexpected spike after a meal, these timely alerts ensure timely action.
- Reduced Frequency of Fingerstick Tests: Traditional monitoring often requires multiple fingersticks throughout the day, which can be painful and inconvenient. CGM systems drastically cut down or, in some cases, eliminate the need for these manual checks, making the monitoring process more comfortable. The American Diabetes Association has discussed the benefits of CGM systems in greater detail.
- Comprehensive Data Collection: With the ability to capture blood glucose data every few minutes, CGM devices amass a wealth of information over days, weeks, and months. This extensive record can be invaluable during consultations with healthcare providers, helping fine-tune management strategies.
- Enhanced Decision Support: Some advanced CGM systems offer decision support features, suggesting potential insulin doses or dietary adjustments based on current readings and trends. This can be particularly helpful for those unfamiliar with managing blood sugar fluctuations.
- Peace of Mind: Knowing that they’re constantly monitored offers immense psychological relief to many individuals with gestational diabetes. It instills confidence in their daily routines and reduces anxiety associated with potential blood sugar abnormalities.
- Improved Overall Health Outcomes: Regular and proactive management with CGM has shown to improve gestational diabetes outcomes, reducing risks like high blood pressure in the mother and respiratory distress syndrome in the baby.
The introduction of CGM in diabetes care, especially in managing conditions like gestational diabetes, has been nothing short of transformative. Offering a blend of convenience, comprehensive data, and advanced features, it’s a powerful tool in the quest for optimal blood sugar management and a healthy pregnancy.
In the constantly evolving landscape of diabetes care, Aptiva Medical remains a beacon of innovation and reliability. Their CGM offerings not only simplify the management of gestational diabetes but also play a pivotal role in ensuring healthier pregnancies and better long-term outcomes for both mother and baby.

The Future and Prevention
As we stand at the crossroads of medical advancements and increasing awareness, the narrative around gestational diabetes is shifting. It’s not just about management, but also about anticipation and prevention. By understanding the broader horizon of this condition and looking towards the future, we can shape a more informed and proactive approach.
- Promising Research and Developments: The medical community is continually delving deeper into the intricacies of gestational diabetes. Recent studies are examining genetic markers, the influence of gut microbiota, and environmental factors. The insights from these studies can pave the way for more precise prediction models and innovative therapeutic interventions.
- Pre-Conception Counseling: Recognizing that prevention can start even before conception, as suggested by Johns Hopkins Medicine, healthcare professionals are advocating for pre-conception counseling. Women with higher risk factors like polycystic ovary syndrome or a history of diabetes are being guided on maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet.
- Enhanced Prenatal Screening: With the advancement in diagnostic tools, future prenatal screening methods may detect gestational diabetes even earlier, facilitating timely interventions and potentially reducing adverse pregnancy outcomes.
- Dietary and Lifestyle Interventions: A focal point of prevention lies in understanding the profound impact of diet and lifestyle. Initiatives are being developed to promote eating healthy foods and maintaining an active lifestyle among pregnant people. This not only helps in keeping blood sugar levels in a healthy range but also contributes to overall health.
- Community Support and Awareness: Building community support systems can play a crucial role in prevention. Peer-led groups, workshops, and awareness campaigns can help women understand the risk factors, promote early diagnosis, and foster healthier lifestyle habits.
- Post-Pregnancy Follow-up: It’s essential to acknowledge that the risk doesn’t end once the baby is born. Women who’ve had gestational diabetes have a heightened risk of developing type 2 diabetes later in life. Regular follow-ups post-pregnancy, glucose tolerance tests, and lifestyle recommendations can help in long-term health monitoring.
- Harnessing Technology: With the rapid strides in technology, the future might see more wearable devices, AI-driven prediction tools, and personalized medicine approaches, all geared towards early detection, seamless management, and robust prevention of gestational diabetes.
- Societal and Policy Changes: At a macro level, policies can shape a society’s health trajectory. Initiatives to promote healthier foods, curb the sale of ultra-processed products, and create conducive environments for physical activity can indirectly contribute to reducing gestational diabetes incidences.

The future of gestational diabetes care intertwines prevention with empowerment. By equipping women with knowledge, resources, and the right tools, we move closer to a future where gestational diabetes can be more effectively anticipated, managed, and perhaps, even prevented.
Gestational diabetes, while transient in its nature, casts a significant imprint on both maternal and infant health. With an intricate web of physiological processes, risk factors, and potential outcomes, it beckons for more than just fleeting attention. It demands a comprehensive, enlightened approach. By demystifying the complexities surrounding this condition, we not only enable better management for those currently affected but also kindle hope for a future where its incidence might be substantially diminished.
Today, with the power of technology and continuous glucose monitoring, coupled with companies like Aptiva Medical at the forefront, we are undoubtedly better equipped than ever before to monitor and manage this condition. But it’s imperative to remember the equal, if not greater, significance of awareness, timely diagnosis, and preventive measures. These efforts reflect a collective endeavor to not just address the immediate concerns but to envision a healthier trajectory for generations to come.
As the discourse around gestational diabetes evolves, so should our strategies. Rooted in science, propelled by innovation, and anchored by community and individual resilience, the journey towards understanding, managing, and eventually diminishing the impact of gestational diabetes is a shared one. It’s a testament to the power of knowledge, the potential of technology, and the indomitable spirit of mothers everywhere, striving for a healthier tomorrow for themselves and their children.