Continuous glucose monitors and their related supplies are covered by Medicare. Diabetes affected an estimated 13% of persons in the United States in 2018. This figure increased to 26.8 percent among persons aged 65 and up. CGM devices substitute blood sugar monitoring that can be used to make diabetes treatment recommendations such as dietary changes or insulin administration adjustments. If you have diabetes and are on Medicare, you may wonder, “Does Medicare cover continuous glucose monitors (CGM)?” The excellent thing is that certain CGM devices are covered, as long as you meet the Medicare coverage guidelines. Continue reading this article to find out what the criteria are, as well as other important information regarding continuous glucose monitoring.
Is Continuous Glucose Monitoring Covered by Medicare?
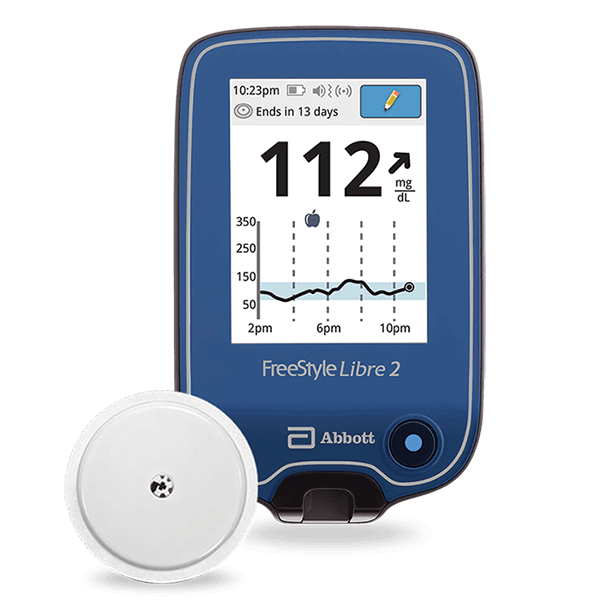
In most situations, Medicare will cover the monthly products for a monitor, which may include sensors, transmitters, and batteries according to the manufacturer. Even though devices are covered, consumers may be required to pay medical costs or taxes. Because Medicare Supplement must offer a similar level of treatment as Original Medicare, some or all of the costs may also be covered for those with supplemental Healthcare Insurance Plan policies. Independent Insurances, on the other hand, may have varied regulations regarding costs, brands, and where you can access services. Continuous glucose monitors were previously considered preventative rather than medically required, limiting the number of individuals who could be covered for CGM devices. However, in 2021, the policy changed, enabling more of the population to benefit from the use of these devices to help manage their condition.
Who Is Eligible for Continuous Glucose Monitors Covered by Medicare?
Continuous glucose monitoring is usually only covered for people diagnosed with diabetes who inject insulin daily. This includes patients with Type 1 diabetes as well as some type 2 diabetics. The monitors are meant to help patients with diabetes self-management who must constantly change their medications. Patients who do not inject insulin 3 or more times per day are typically not covered under Medicare or Private insurance guidelines. It’s also not covered for people who take non-insulin medications to manage their diabetes. Your doctor or Aptiva Medical CGM specialist will be able to tell you if you fit the Medicare eligibility.
What is required to be eligible for Medicare CGM coverage?
There are a few requirements for receiving Medicare coverage for a Continuous Glucose Monitor:
- The beneficiary has diabetes mellitus and,
- The beneficiary is insulin-treated with multiple (three or more) daily administrations of insulin or a Medicare-covered continuous subcutaneous insulin infusion (CSII) pump; and,
- The beneficiary’s insulin treatment regimen requires frequent adjustment by the beneficiary on the basis of blood glucose monitor (BGM) or CGM testing results; and,
- Within six (6) months prior to ordering the I-CGM, the treating practitioner has an in-person visit with the beneficiary to evaluate their diabetes control and determined that criteria (1-3) above are met; and,
- Routine recommended follow-up care is expected.
How Can I Obtain a Low-Cost Continuous Glucose Monitor?
Individuals who do not qualify for a continuous glucose monitor through Medicare may still be able to obtain a low-cost device. To begin, check your health insurance policy to determine if monitors are covered. If your health insurance does not cover a monitor, you might try contacting the providers. Many companies provide financial support to qualifying clients to help them gain access to monitoring technology, such as free trials and continued supply reductions.
Is Medicare going to cover extra Diabetic products?
Medicare covers various diabetes products such as testing kits, conventional blood glucose monitors, infusion pumps, and management expertise. Diabetes-related knee problems may also likely require the use of medicinal shoes. Insulin and other glucose-controlling drugs may also be covered by Medicare, but only as part of prescription coverage.