What you can do to reduce your risk factors
A diabetic coma is a sustained loss of consciousness caused by complications of diabetes – primarily high or low blood sugar. A diabetic coma patient is alive but unconscious. They can’t respond deliberately to stimuli. A diabetic coma is a medical emergency that can result in permanent brain damage and death.
Learn the causes, symptoms, and ways to prevent a diabetic coma by reducing your risk factors and improving your type 1 diabetes management.
What causes diabetic coma?
Diabetic Ketoacidosis
Diabetic Hyperosmolar Syndrome
Hypoglycemia
Diabetic Ketoacidosis (DKA)
Your body breaks down the food into glucose, your body’s primary source of energy. Insulin from your pancreas allows glucose to enter your cells and be used. Extra glucose is stored in your liver and muscles as glycogen.

When you don’t eat, your blood sugar drops, and you stop producing insulin. Your pancreas releases a different hormone – glucagon – telling your liver to break down stored glycogen and release glucose into your blood. In a non-diabetic body, this is how blood sugar levels are regulated.
If you don’t eat for a long time, your body will break down fat to produce an alternative fuel – ketones. This is a safe and natural process known as ketosis.
For those with diabetes, those who are starving, or those who struggle with alcohol addiction, ketosis can quickly lead to diabetic ketoacidosis – a toxic level of ketones that turns the blood acidic.
For people with diabetes, ketoacidosis is not typically caused by dieting. It occurs when there’s not enough insulin to turn glucose into energy. The body responds as if the carbs were never consumed.
Symptoms and potential complications of diabetic ketoacidosis include:
Hypokalemia (low potassium)
Cerebral Edema (brain swelling)
Pulmonary Edema (fluid in lungs)
Kidney damage
Other organ damage
Fluid loss
Vomiting
Dehydration
Fruity breath odor
Labored breathing
Hyperventilation
Rapid heartbeat
Confusion/disorientation
Coma
Thirst
Frequent urination
Blurred vision
Weakness
Fatigue
Headache
Nausea
Shortness of breath
Stomach pain
Dry mouth
Diabetic Hyperosmolar Syndrome
Hyperosmolar hyperglycemic state or syndrome refers to blood glucose levels above 600 mg/dL or 33.3 mmol/L. When the blood sugar is that high, the extra glucose is filtered as waste, causing frequent urination and the rapid loss of fluids. Untreated, diabetic hyperosmolar syndrome can cause life-threatening dehydration.
Hyperosmolar syndrome is classified by the absence of ketones. High blood glucose levels with ketones are classified as ketoacidosis.
Hypoglycemia
Your brain and other organs require glucose to function. If you don’t consume enough, you experience low blood sugar, otherwise known as hypoglycemia. Severe hypoglycemia might cause you to pass out and/or enter a diabetic coma.
High insulin levels can also cause low blood sugar. The insulin causes your cells to absorb too much of your blood sugar and signal your liver to stop producing blood sugar. The result is the same as if you didn’t consume enough. The same effect can be caused by too much alcohol consumption or exercise.
Hypoglycemia is the most common cause of diabetic coma.
Hypoglycemia (low blood glucose levels)
Most people should have a fasting blood sugar of at least 70 mg/dL or 3.9 mmol/L. Anything below that is hypoglycemia. Your doctor can give you a more accurate threshold for what’s healthy for your body.
Unless your doctor tells you otherwise, you should immediately treat yourself for blood sugar below 70 mg/dL. Immediate treatment is to get your blood sugar within a healthy range as fast as possible with a high-sugar food, drink, or medication.
Long-term treatment requires identifying and treating the cause of your low blood glucose levels.
The most common cause of hypoglycemia is diabetes medication.
Causes
Diabetes is a condition that prevents insulin from doing its job – either because your body doesn’t produce enough or because your body doesn’t respond to it. Type 1 diabetes is a production issue, and type 2 diabetes is a responsivity issue. (In this article, we address type 1 diabetes specifically.)
The lack of insulin causes glucose to build up in your bloodstream, unable to enter your cells and be used for energy. Insulin injections, pumps, or other medications can help correct the problem and lower your blood sugar.
Too much corrective medication can cause your blood sugar to drop quickly and dramatically, causing hypoglycemia. You might also experience hypoglycemia if you eat less or exercise more than usual.
Reactive Hypoglycemia (postprandial hypoglycemia)
Reactive hypoglycemia is low blood glucose caused by a meal. It happens most often in patients who have had surgery that interferes with their stomach function, most commonly bypass surgery.
Symptoms and Potential Complications
Seizure
Coma
Death
Dizziness
Weakness
Falls
Injuries
Car accidents
Dementia
Paleness
Shakiness
Sweating
Headache
Hunger
Nausea
Irregular heartbeat
Fatigue
Irritability
Anxiety
Difficulty concentrating
Lightheadedness
Tingling
Numbness
Confusion
Unusual behavior
Loss of coordination
Slurred speech
Blurry vision
Tunnel vision
Nightmares
Hypoglycemia Unawareness
If you’ve had diabetes for a long time, you might experience a condition called hypoglycemia unawareness, meaning your blood glucose level can drop without warning symptoms. That’s why it’s vital to monitor your blood sugar constantly, even if you’re not experiencing symptoms.
Hyperglycemia (high blood glucose levels)
High blood glucose occurs when your body has too little insulin to regulate and transport glucose. Hyperglycemia typically refers to any fasting blood sugar level above 125 mg/dL or a blood sugar level above 180 mg/dL one to two hours after eating. These levels are also indications of diabetes mellitus.
Symptoms and Potential Complications
Nerve damage
Damage to blood vessels
Tissue damage
Organ damage
Heart attack
Stroke
Eye damage
Impaired healing
Ketoacidosis
Coma
Death
High blood glucose
Thirst
Hunger
Blurred vision
Frequent urination
Headache
Fatigue
Weight loss
Vaginal infections
Skin infections
Impaired healing
Causes
Hyperglycemia is typically the result of an imbalance between insulin levels and glucose levels. Your dose might not be right for your needs, or you’re not maintaining the diet you and your doctor agreed on.
Your blood sugar levels can rise if you’re sick or less active than usual. And just like physical stress, emotional stress can contribute to hyperglycemia, as well as:
Endocrine conditions
Pancreatic disease
Diuretics and steroids
Other medications
Surgery or physical trauma
Double Diabetes
People with type 1 diabetes (poor insulin production) can develop type 2 diabetes (insulin resistance or insulin delivery problems). If you develop type 2 diabetes, your insulin injections will no longer be as effective. Talk to your doctor immediately if you think your insulin is less effective than it used to be.
The Dawn Phenomenon

Every morning around 4 AM, our bodies produce a surge of hormones – even those without diabetes. Dawn phenomenon hormones include hGH, cortisol, and glucagon. These hormones stimulate the release of glucose from your liver into your bloodstream.
Some people with type 1 diabetes can’t respond adequately to the dawn phenomenon on their own, so their blood sugar levels rise every morning, and they might wake up with hyperglycemia.
How to reduce your risk of diabetic coma
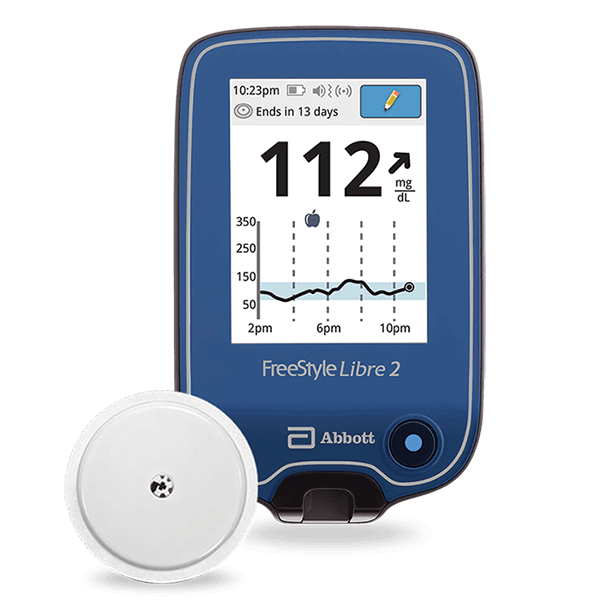
Make management easier with technology
Insulin pump – delivers the set dosage at the set times so you never miss a dose
Continuous Glucose Monitor – monitors your blood sugar all day and night
Artificial Pancreas – monitors your blood sugar and delivers insulin when needed
At-home testing kits (fingerprick tests) – tell you your current blood glucose
(Check your equipment for accuracy by comparing your results with your doctor’s in-office.)
Monitor your blood sugar after any unusual food or activity
Every food, substance, and activity has an effect on your blood sugar level. Monitor your blood glucose carefully after exercise, eating, drinking, sleeping, and especially during and after any sort of trauma. Physical trauma can include illness, injury, surgery, stress, etc.
Talk about weight loss and eating habits with your doctor
Some T1D patients are tempted to deliberately skip meals and insulin doses in an attempt to lose weight. Weight management is important to your overall health, but this approach is dangerous and life-threatening. It significantly increases your risk of diabetic coma.
Avoid alcohol
Alcohol poses a danger in two ways. First, it can have unpredictable effects on your blood glucose levels, increasing your risk for life-threatening complications.
Second, the effects of alcohol on your cognition and your body make it difficult to identify symptoms of hypoglycemia. If your blood sugar drops while you’re drinking and you don’t notice the symptoms or attribute them to intoxication, your condition will quickly become critical.
Avoid narcotics, illegal drugs, drug abuse, and psychotropic substances

Drugs – even over-the-counter medications – can cause severe low blood sugar levels and severe high blood glucose levels. As with alcohol, your condition may inhibit your ability to identify symptoms, causing diabetic coma or mortality.
How to prevent diabetic comas
Continuous Glucose Monitor (CGM)
By the time you have symptoms – if you have symptoms – your blood glucose will already be out of range. A Continuous Glucose Monitoring system can help you track your blood sugar throughout the day and night without constantly pricking your fingers.
CGM is also known to improve your time in range (TIR), which reduces your risk of complications like hypoglycemia, brain damage, organ failure, and diabetic coma.
Continuous Glucose Monitors are wearable devices that track your glucose levels in real time with tiny filaments that are inserted just under the skin. The data is sent to a receiver or to your mobile device.
By tracking constantly, you can identify trends in your blood sugar levels and learn how your body reacts to different activities and substances. The monitor can alert you when your blood sugar is in danger of getting out of range.
When you receive an alert, it’s important to verify the data with a blood glucose test (fingerprick test).
CGM systems are more expensive than other monitoring methods, but your insurance (especially Medicare) might cover the entire cost.
Insulin pump
An insulin pump operates based on your programmed schedule or is combined with a CGM system to create an “artificial pancreas” that doses your insulin based on your real-time glucose readings. On its own or as part of an artificial pancreas, an insulin pump can increase your time in range, decrease missed doses and dosing errors, and reduce your risk of diabetes complications.
Seek medical care
when your blood sugar is over 250 mg/dL or 14 mmol/L, test yourself for ketone levels – if your ketone level is high, call your healthcare provider
if you have any ketones present in your urine and are vomiting, contact your provider or go to the ER immediately
Talk to your doctor about…
how to respond to an emergent blood sugar level
how to manage your blood sugar if you get sick and can’t eat normally
Stay stocked up on…
one week of diabetes supplies
extra glucagon kit
fast-acting sugar sources
glucose tablets
More tips for preventing a diabetic coma
Eat light snacks and meals throughout the day.
Check your blood sugar frequently or employ a CGM system.
Check blood sugar when you’ve exercised, eaten, or done any unusual activity.
Always take your medication as directed by your doctor.
Review and adjust your treatment plan regularly.
If you drink, drink with extreme caution, and a meal.
Teach the people around you how to recognize symptoms of hypoglycemia or hyperglycemia and how to administer emergency injections.
Wear a medical identification necklace or bracelet.