Can a Continuous Glucose Monitoring (CGM) System achieve better outcomes for people with diabetes mellitus?
Change is scary for some people, especially when you’ve been doing things the same way for years. You’ve been jabbing your fingers for so long they hardly even hurt anymore. Why switch it up now? Well, it turns out there are much bigger benefits to continuous glucose monitoring (CGM) than saving your fingertips.
When you can see your data in real-time, you can prevent blood sugar issues before you feel any symptoms. You can review your trends to optimize your treatment and live a healthier, happier life. And you might even be able to get a CGM device for free.

CGM Benefits at a Glance
Continuous glucose monitoring requires virtually zero fingersticks.
Make proactive treatment decisions by seeing your blood sugar before symptoms.
Get more insight into your blood glucose level trends with recorded data.
Improve your health and experience a better quality of life.
Medicare covers CGM for those who qualify.

What is continuous glucose monitoring?
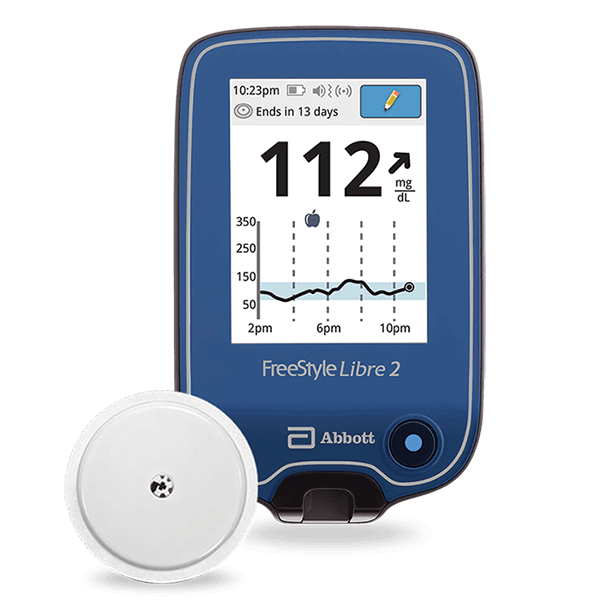
Your current blood glucose monitoring regimen probably feels pretty “continuous,” having to jab your fingers and use test strips several times a day. Continuous glucose monitoring is much more hands-off. A small sensor with an adhesive pad sticks to your skin with a small wire catheter inserted just deep enough to take continuous readings.
On the front of the sensor, you’ll attach a small transmitter. The transmitter sends the data to your smart device or the receiver that comes with the monitoring kit. That’s it—no poking your fingers and sticking strips into a testing device over and over. You wear the monitor continuously and get better control over your health. You can even bathe and swim with more advanced CGM devices like the Dexcom G6.
How does a continuous glucose monitor work?
Your CGM system will come with an applicator. Every model is different, but the instructions usually look something like this:
clean an area on your arm or abdomen with an alcohol wipe to remove oils
let the alcohol dry while you put the new sensor in the applicator
place the applicator on the cleaned area and push down on the device or button
connect the transmitter to the sensor by pressing it into place
use the included receiver or your smartphone to begin monitoring your glucose levels
The applicator places the needle sensor into the subcutaneous adipose tissue (fat tissue under the skin), where it can contact the interstitial fluid between your cells, which delivers oxygen and nutrients from your capillaries. Then, the sensor measures your interstitial glucose levels.
The sensor sends that data through the transmitter to your receiver or smart device, where you can use your glucose trends to make better diabetes treatment decisions.
How accurate are continuous glucose monitors?
The accuracy of certain meters is tested by determining the MARD – mean absolute relative difference. MARD measures the difference between a meter’s result and the corresponding laboratory measurement.
A MARD less than 10% is considered “good analytical performance.” Clinical data for the Dexcom G6 – one of the most popular CGM systems – shows a MARD of 9%, and the sensors maintain that MARD over the time they’re worn.
CGM has proven so accurate that medical professionals consider it a better metric for therapeutic decisions. A 2017 German study revealed that it might be “risky from a therapeutic point of view to use blood glucose for therapeutic decisions.”
They conclude that “it may be reasonable to abandon blood glucose measurements as the basis for diabetes management and switch to using ISF glucose as the appropriate therapeutic target.”
Sidenote: Keep in mind therapeutic targets are different than acute treatment. You should always check your blood sugar before responding to a dip or spike reported by your CGM device. And talk to your doctor before making any changes to your insulin regimen.
How is an “interstitial glucose level” different than blood glucose levels?
Glucose moves from your blood to your interstitial fluid (ISF) via the capillaries, but not all of it gets there. The glucose that does get there can hang around for a while. So when you have high blood sugar, your ISF glucose will probably be lower. When you have low blood glucose, your ISF glucose will probably be higher.
Remember:
Your glucose numbers from a blood glucose meter and an ISF glucose meter never need to be the same.
The difference between the two will be greatest when your sugar levels change quickly.
Before treating a high or low ISF reading, you should always use a blood glucose meter. It isn’t that the ISF could be wrong, but that you need to know how much glucose is in your blood before making diabetes treatment decisions.

What are the benefits of a CGM system?
Continuous glucose monitoring (CGM) isn’t just the next popular thing. It is truly a better glucose reading system for most people with type 1 diabetes. Knowing your blood glucose levels ahead of time can completely change your treatment approach from reactive (damage control) to proactive (prevention).
Around-the-Clock Blood Glucose Readings
A traditional blood glucose meter is an invaluable tool compared to blind treatment, but medical technology has grown. Continuous monitoring gives you a complete picture day and night. You and your healthcare provider can clearly see how food, physical activity, and other factors affect your body. Then, together, you can optimize your treatment plan.

Fewer Fingersticks
Advanced CGM devices like the Dexcom G6 use tiny sensor catheters inserted just under the skin to monitor glucose levels without fingersticks. Your CGM system will include three simple components that operate continuously: a sensor, a transmitter, and a receiver or smart device.
Proactive Treatment Decisions
Customize your blood glucose level thresholds and receive alerts when your glucose readings are out of your target range. Knowing you need treatment before you feel symptoms can prevent the blood sugar levels that pose a severe threat to diabetes patients.
Lower A1C
Your A1C averages your blood glucose levels over the past few months by measuring what percentage of hemoglobin proteins in your blood are glycated (coated in sugar). A continuous glucose monitor might help you lower your A1C, reducing your risk of diabetes complications like digestive and kidney diseases.
CGM Works for Injections or Your Insulin Pump
Your CGM device will work whether you do your own insulin injections or use an insulin pump. If you use an insulin pump, you’ll continue to use it the same way. If your continuous glucose monitor alerts and you confirm your current blood sugar with a blood glucose meter, you can administer a bolus dose as you normally would. Analyzing your blood sugar trends can help you and your healthcare professionals optimize your insulin pump therapy.

More Insight into Your Blood Sugar Trends
A 2016 review of self-monitoring of blood glucose (SMBG) presents evidence that CGM is a more effective monitoring method for insulin-dependent diabetes mellitus. CGM devices help prevent hypoglycemia and hyperglycemia by recording the speed and direction of changes in glucose levels. They give you a more complete picture, eliminate missed testing intervals, and alert you at customized thresholds.
Better Glucose Control
Diabetes treatment is all about controlling your glucose. Without adequate control, serious health complications can occur, even if you don’t become severely hypo or hyperglycemic. The goal is to avoid the big swings, and CGM lets you do that without letting diabetes take over your life.
You get continuous feedback about how your diet and activity level affects your body. With that information, you can optimize your treatment regimen and how much insulin you administer. Be sure to discuss any significant changes to your treatment with your doctor first.
Better Overall Health and Wellness
We all just want to be well. We want convenience, freedom, and control. And that starts with getting your A1C within range. A CGM system can help you achieve fewer low blood sugar readings and do other things with your time besides having diabetes.
What does the American Diabetes Association say about continuous glucose monitoring?
“CGMs provide users with real-time, dynamic information about their [blood sugar] levels around the clock and alerts to prevent dangerous high or low glucose levels, leading to better diabetes management and ultimately improved health outcomes.” And they’re not the only ones.
The Endocrine Society recommends CGM for those with A1C above 7%, the typical goal for type 1 diabetes. In 2017, the Journal of Diabetes Science and Technology published a study that concluded the use of CGM facilitated greater A1C improvements and reduced healthcare system use compared to SMBG use, regardless of how the patients administer insulin.
The National Institute of Diabetes and Digestive and Kidney Diseases explains that a CGMS can help you “better manage your glucose levels” and “have fewer low blood glucose emergencies.”

What are the disadvantages of CGM?
Ultimately, your decision to switch to a CGM system is between you and your healthcare professional. Like every other glucose data solution, CGM systems have their reported drawbacks. Consider the downsides, and then click the button to learn if your insurance will cover your CGM device.
Discomfort During Initial Insertion
Some people report pain during the initial sensor insertion. Diabetes Technology & Therapeutics published a study in 2018 in which 84% of participants reported no pain to mild pain when using an auto-applicator. All participants said the applicator was easy to use. There is no pain after the initial insertion if completed successfully.
Lost Signal Means Gaps in Your Data
If the signal between the sensor and transmitter or transmitter and receiver is lost, there will be a gap in your data. This is an unfortunate risk with any device that relies on a wireless signal. However, the amount of data you receive from a CMGS will still be vastly higher than traditional methods, even if you have occasional gaps.
Adhesives Can Cause Irritation
Some users have reported an allergic reaction to the adhesive on the sensors of some CGM devices. Even without allergies, it’s possible to have skin irritation around the adhesive pad, especially if you wear it past the recommended time limits.
Fun fact: a study in the National Library of Medicine tested patients who thought they had an allergy to medical adhesive. Their results showed 15% of allergic reactions were caused by a different substance, and 73% had irritant (not allergic) contact dermatitis after leaving the bandage on for seven days.
There were no genuine allergic reactions to medical adhesive detected.

You Have to Change Your CGM Sensor
Due to the nature of the sensor and the skin irritation issue, you have to replace your sensor in a new location periodically. The frequency depends on which CGM system you use. The more advanced models can stay on for approximately two weeks.
Sensor swaps might be considered a downside, but you should consider the alternatives when deciding what’s right for you. When you compare a fortnightly schedule to fingersticks several times a day, changing a sensor doesn’t seem intolerable.
Your CGM System Can’t be Recycled
The world is becoming more eco-conscious every day, and thank goodness! Given some time, CGM systems may become recyclable, but as of today, they are not. The good news is that you’ll only need to throw away the sensor. The applicator, transmitter, and receiver are good for the long term.
Some People Don’t Want to Wear a CGM Sensor
For some people, it comes down to simply not wanting to wear a sensor on their body. This aversion is typically seen in people with new-onset type 1 diabetes who aren’t yet comfortable with the intensive regimen they’ll have to maintain.
Adolescents between the ages of eight and 18 are also more reluctant than other age groups to wear their sensors because of the social stigma they perceive.

Optional Alarms Can be Disruptive
If you set ambitious thresholds or if your blood sugar frequently fluctuates beyond your goal range, the alerts from your device might become irritating or disruptive. This is especially true for those who spend most of the day working in an office setting or somewhere quiet.
However, considering the alternative is not knowing that your blood sugar is trending out of range, it’s probably worth it to have your activities interrupted with an alert about your health. Over time, CGM can help you stay in range for more of the day, so you should hear fewer alarms as you continue to wear it.
CGM Data Can be Overwhelming
If you’re used to traditional testing, you might feel overwhelmed with the new data you receive. The CGM system doesn’t measure blood glucose. CGM measures glucose found in fatty tissue with a tiny sensor inserted just under the skin. So first, you’ll have to get used to interpreting the new metric.
Next, you’ll learn to watch your trends and optimize your lifestyle and treatment. If you feel overwhelmed, take it slow and master one bit of information at a time. Don’t forget to tell your doctor about your progress.

Self-Pay Costs Can be Prohibitive
The newest thing is always the most expensive. Fortunately, insurance companies understand the preventative benefits of using continuous glucose monitoring to manage type 1 diabetes. Those with Medicare can typically get their devices without paying anything out of pocket.
Order through Aptiva Medical to find out if you qualify for full coverage. Then you can choose the CGM system you want with the help of a knowledgeable support agent. Once you decide, Aptiva works with your insurance company and delivers to your door at no cost to you.